Discover What Really Causes Autoimmune Diseases—and How to Reduce Your Risk
Autoimmune diseases are a complex category of disorders where the body's immune system mistakenly targets its own tissues, leading to inflammation and damage. The increasing prevalence of these diseases has sparked considerable interest in understanding their underlying causes. Key risk factors contributing to autoimmune diseases include genetic predispositions, environmental triggers, and immune system imbalances. By exploring these factors, individuals can gain insight into the development of these conditions and adopt effective strategies for managing risks and prevention. This article delves into the intricacies of these risk factors, offering a comprehensive overview to help individuals make informed health decisions.
Autoimmune diseases represent a significant health challenge, affecting approximately 50 million Americans according to various health organizations. These disorders encompass more than 80 different conditions, including rheumatoid arthritis, lupus, multiple sclerosis, type 1 diabetes, and celiac disease. While medical science has made considerable progress in treating these conditions, understanding their root causes remains an evolving area of research. By examining the interplay between genetics, environmental factors, and immune system function, we can better grasp how these diseases develop and what steps might help reduce risk.
What Are Autoimmune Diseases and How Do They Develop?
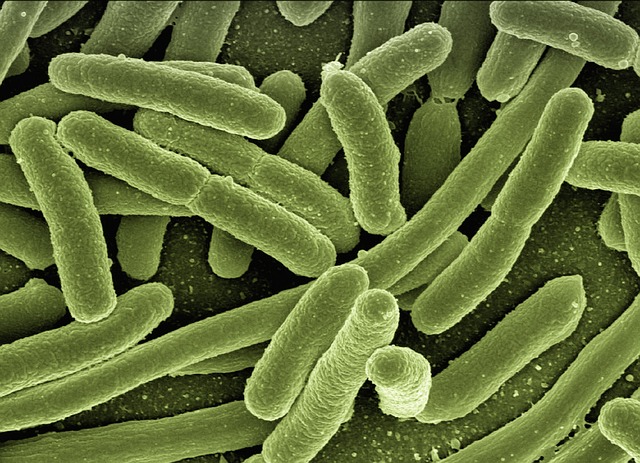
Autoimmune diseases occur when the body’s immune system fails to distinguish between foreign invaders and its own healthy tissues. Normally, the immune system protects us from bacteria, viruses, and other harmful pathogens. However, in autoimmune conditions, this defense mechanism becomes misdirected, producing antibodies that attack the body’s own cells, organs, and tissues.
The development of autoimmune diseases typically involves a breakdown in immune tolerance—the process by which the immune system learns to recognize self from non-self. This breakdown can affect various parts of the body, leading to organ-specific conditions like Hashimoto’s thyroiditis, which targets the thyroid gland, or systemic conditions like lupus, which can affect multiple organ systems simultaneously. The resulting inflammation and tissue damage cause the diverse symptoms associated with these disorders, ranging from fatigue and joint pain to more severe complications affecting vital organs.
How Do Genetic Factors Influence Autoimmune Disease Risk?
Genetics play a substantial role in autoimmune disease susceptibility. Research has identified numerous genes associated with increased risk for various autoimmune conditions. The human leukocyte antigen (HLA) gene complex, which helps the immune system distinguish between the body’s own proteins and foreign substances, shows particularly strong associations with autoimmune diseases.
However, genetics alone do not determine whether someone will develop an autoimmune condition. Studies of identical twins show that if one twin has an autoimmune disease, the other twin’s risk is elevated but not guaranteed—typically ranging from 15 to 50 percent depending on the specific condition. This indicates that while genetic predisposition creates vulnerability, other factors must also be present for disease to manifest. Family history remains an important risk factor, with individuals having a first-degree relative with an autoimmune disease facing higher odds of developing similar or related conditions.
What Environmental Factors Trigger Autoimmune Responses?
Environmental triggers serve as critical catalysts in autoimmune disease development, particularly in genetically susceptible individuals. Infections represent one of the most studied environmental factors. Certain viral and bacterial infections can trigger autoimmune responses through molecular mimicry, where microbial proteins resemble human proteins, confusing the immune system. Epstein-Barr virus, for example, has been linked to multiple sclerosis and lupus development.
Chemical exposures also contribute to autoimmune disease risk. Cigarette smoking has been strongly associated with rheumatoid arthritis and lupus, while exposure to certain solvents, pesticides, and industrial chemicals may increase susceptibility. Additionally, dietary factors have gained attention, with research suggesting that high salt intake, processed foods, and changes in gut bacteria composition may influence immune system function. Vitamin D deficiency has been observed in many autoimmune disease patients, though whether this is a cause or consequence remains under investigation. Geographic patterns in autoimmune disease prevalence support the environmental hypothesis, with certain conditions appearing more frequently in specific regions or populations.
How Do Immune System Imbalances Lead to Autoimmune Conditions?
The immune system maintains a delicate balance between activation and regulation. Regulatory T cells normally suppress immune responses to prevent attacks on the body’s own tissues. In autoimmune diseases, this regulatory function becomes impaired, allowing self-reactive immune cells to proliferate and cause damage.
Several mechanisms contribute to immune system imbalances. The gut microbiome—the trillions of bacteria living in our digestive tract—plays an increasingly recognized role in immune regulation. Disruptions to this microbial community, whether from antibiotics, diet, or other factors, may compromise immune tolerance. Hormonal influences also affect immune function, which may explain why women develop autoimmune diseases at significantly higher rates than men, with some conditions showing a female-to-male ratio of 9:1. Chronic stress and sleep deprivation can dysregulate immune responses, potentially contributing to autoimmune disease development or flare-ups in those already diagnosed.
What Strategies Help Manage Risk and Support Prevention?
While autoimmune diseases cannot always be prevented, certain lifestyle modifications may help reduce risk or delay onset in susceptible individuals. Maintaining a balanced, anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids supports overall immune health. Some individuals find that identifying and avoiding specific food triggers, such as gluten in celiac disease, proves essential.
Regular physical activity helps regulate immune function and reduce chronic inflammation. Stress management techniques including meditation, yoga, and adequate sleep support healthy immune system balance. Avoiding smoking and limiting exposure to known environmental toxins represents another important preventive measure. For those with family history or early symptoms, working closely with healthcare providers for monitoring and early intervention can improve outcomes. Some research suggests that maintaining healthy vitamin D levels through sensible sun exposure or supplementation may provide immune benefits, though this should be discussed with a healthcare professional.
Early detection remains crucial, as prompt treatment can prevent irreversible damage in many autoimmune conditions. Individuals experiencing persistent unexplained symptoms such as chronic fatigue, joint pain, skin changes, or digestive issues should seek medical evaluation. While we cannot control genetic factors, understanding modifiable risk factors empowers individuals to make informed health decisions that may influence their autoimmune disease risk trajectory.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




